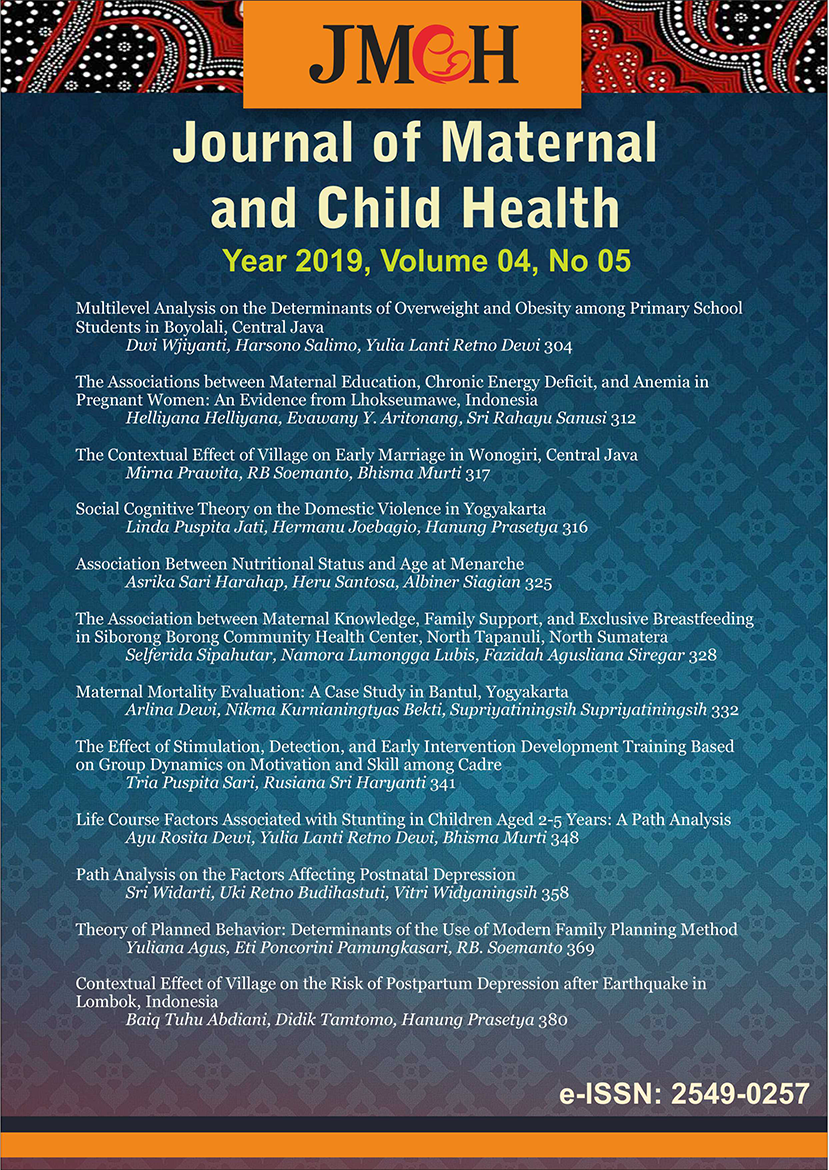
Life Course Factors Associated with Stunting in Children Aged 2-5 Years: A Path Analysis
Abstract
Background: Worldwide, in 2014, 23.8% of the children under-five years of age were stunted following the WHO definition, 7.5% were wasted but 6.1% had overweight or were obese. Developing countries host the bulk of the global stunting and child mortality rate.
References
Correai LL, Silva AC, Campos JS, Andrade FMO, Machado MMT, Lindsay AC, Leite AJM, Rocha HAL, and Cunha AJLA(2014). Prevalence and determinants of child undernutrition and stunting in semiarid region of Brazil.
Dinas Kesehatan Kabupaten Tulungagung (2017). Profil Kesehatan Kabupaten Tulungagung. Tulungagung
Fekadu Y, Mesfin A, Haile D, and Stoecher BJ (2015). Factors associated with nutritional status of infants and young children in Somali Region, Ethiopia: A Cross-Sectional Study. BMC Public Health.
Fitri L (2018). Hubungan BBLR dan ASI Ekslusif dengan Kejadian Stunting di Puskesmas Lima Puluh Pekanbaru. Jurnal Endurance. 1(1).
Geberselassie SB, Abebe SM, Melsew YA, Mutuku SM, Wassie MM (2018). Prevalence of stunting and its associated factors among children 6-59 months of age in Libo-Kemekem district, Northwest Ethiopia; Acommunity based cross sectional study. Plos One 13(5): 1-11
Ikatan Dokter Anak Indonesia (2015). Rekomendasi Praktik Pemberian Makan Berbasis Bukti pada Bayi dan Batita di Indonesia untuk Mencegah Malnutrisi. Jakarta: Unit Kerja Koordinasi Nutrisi dan Penyakit Metabolik Ikatan Dokter Anak Indonesia
Kementerian Desa, Pembangunan Daerah Tertinggal, dan Transmigrasi (2017). Buku Saku Desa dalam Penanganan Stunting. Jakarta : Kementerian Desa, Pembangunan Daerah Tertinggal, dan Transmigrasi
Kementerian Kesehatan Republik Indonesia (2011). Keputusan Menteri Kesehatan Republik Indonesia Nomor 1995/MENKES/SK/XII/2010 tentang standar antropometri penilaian status gizi anak. Direktorat Jendral Bina Gizi dan Kesehatan Ibu dan Anak.
____ (2013). Riset Kesehatan Dasar 2013. Jakarta: Badan Penelitian Dan Pengembangan Kesehatan.
____ (2015). Pembangunan Kesehatan Menuju Indonesia Sehat. Rapat Kerja Kesehatan Nasional Regional Tengah Denpasar, 15 Februari 2015.
____ (2016). Gambaran Umum Program Kesehatan dan Gizi Berbasis Masyarakat untuk Mencegah Stunting.
____ (2016). Situasi Balita Pendek. Jakarta : Pusat Data dan Informasi, Kemenkes RI
____ (2017). Pendekatan Program Kesehatan Masyarakat Tahun 2018. Jakarta: Direktur Jenderal Kesehatan Masyarakat, Kemenkes RI
____ (2018). Buku Saku Pemantauan Status Gizi Tahun 2017. Jakarta: Kementerian Kesehatan Republik Indonesia
Kementerian Pemberdayaan Perempuan dan Perlindungan Anak (KPP&PA) (2015). Profil Anak Indonesia 2015. Jakarta : Kementerian Pemberdayaan Perempuan dan Perlindungan Anak (KPP&PA)
Kusumawati E, Rahardjo S, Sari HP (2015). Model pengendalian faktor risiko stunting pada anak usia di bawah tiga tahun. Jurnal Kesehatan Masyarakat Nasional. 9(3): 249-256.
Mgongo M, Chotta NAS, Hashim TH, Uriyo JG, Damian DJ, Stray-Pedersen B, Msuya SE, Wandel M, Vangen S (2017). Underweight, stunting and wasting among children in Kilimanjaro Region, Tanzania; a Population-Based Cross-Sectional Study. Int. J. Environ. Res. Public Health.
Permatasari DF, Sumarmi S (2018). Perbedaan panjang badan lahir, riwayat penyakit infeksi, dan perkembangan balita stunting dan non stunting. Jurnal Berkala Epidemiologi
Roba KT, O
Silva IC, Fran
Tim Nasional Percepatan Penanggulangan Kemiskinan (2017). 100 Kabupaten/ Kota Prioritas Untuk Intervensi Anak Kerdil (Stunting). Jakarta
Torlesse H, Cronin AA, Sebayang SK, Nandy R (2016). Determinants of stunting in Indonesian children: Evidence from a cross-sectional survey indicate a prominent role for the water, sanitation and hygiene sector in stunting reduction. BMC Public Health, hlm. 3-11
Vir SC (2016). Improving women
Zottarelli LK, Sunil TS, Rajaram S (2014). Influence of parental and socioeconomics factors on stunting in children under 5 years in Egypt. Eastern Mediterranean Health Journal