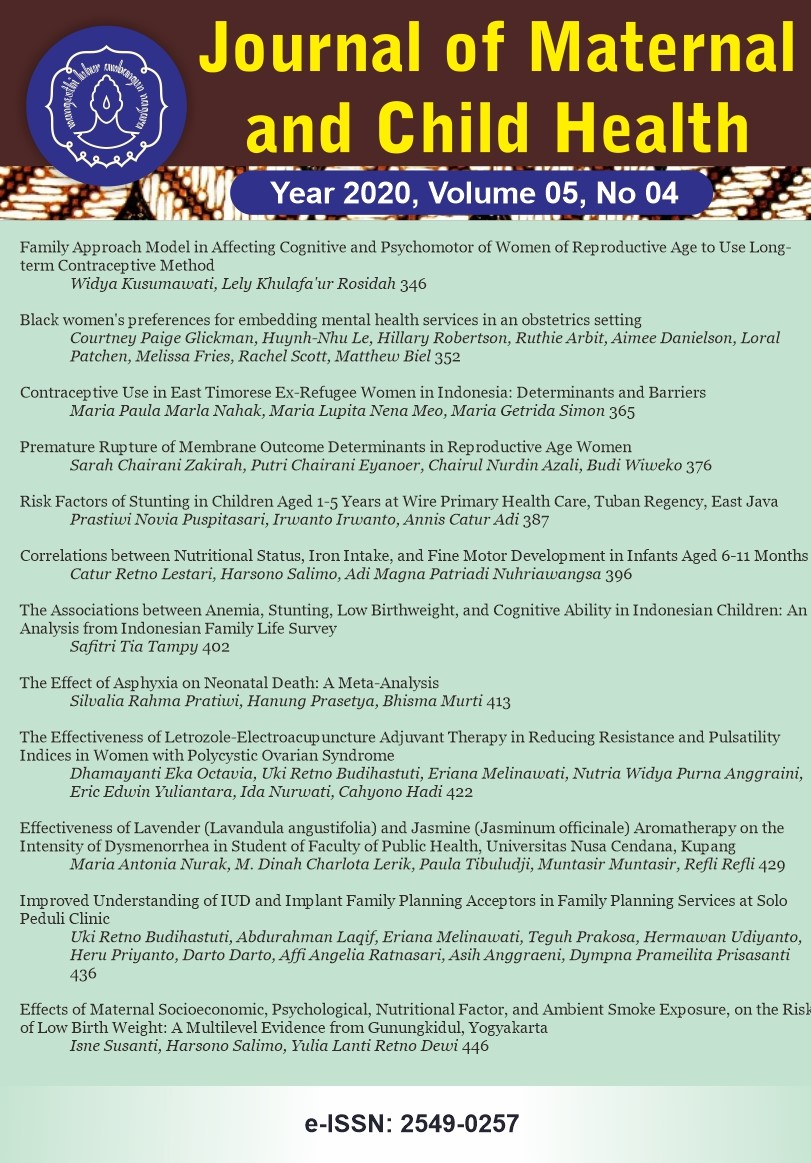
Black women
Abstract
Background: Untreated perinatal depression is a significant public health issue that disproportionately affects low-income black women and may lead to higher maternal mortality rates and disparate birth outcomes. Despite the growing literature documenting prevalence and risk for perinatal depression among black women, our knowledge of patient preferences of mental health interventions in obstetrical (OB) settings among this population is limited. This study explored mental health treatment preferences among black pregnant and postpartum women in an urban OB practice, serving predominantly black women with public insurance.
Subjects and Method: The study sample consisted of 14 perinatal women at an urban obstetrics practice in Washington, DC. Semi-structured interviews were conducted to gain insight into their emotional experiences during pregnancy and postpartum, and to obtain patient recommendations for mental health interventions within an obstetrics setting. Patient interviews were audio-recorded, transcribed, and analyzed by two coders using inductive thematic analysis and consensus procedures.
References
Adouard, F. et al. (2005) Validation of the Edinburgh postnatal depression scale (EPDS) in a sample of women with high-risk pregnancies in France. Archives of Women
Alvidrez, Jennifer (1999) Ethnic Variations in Mental Health Attitudes and Service Use Among Low- Income African American, Latina, and European American Young Women. Community Mental Health Journal. 35 (6), 515
Armstrong, Katrina et al. (2008) Differences in the Patterns of Health Care System Distrust Between Blacks and Whites. Journal of General Internal Medicine. 23 (6), 827
Beeghly, Marjorie et al. (2003) Prevalence, Stability, and Socio-Demographic Correlates of Depressive Symptoms in Black Mothers During the First 18 Months Postpartum. Maternal and Child Health Journal. 7 (3), 157
Braun, Virginia & Clarke, Victoria (2006) Using thematic analysis in psychology. Qualitative Research in Psychology. 3 (2), 77
Byatt, N., Simas, T., Lundquist, R., Johnson, J., & Ziedonis, D. (2012). Strategies for improving perinatal depression treatment in North American outpatient obstetric settings. Journal of Psychosomatic Obstetrics & Gynecology, 33(4), 143
Clever, L., Sarah et al. (2006) Primary Care Patients
Cox, John L et al. (1996) Validation of the Edinburgh postnatal depression scale (EPDS) in non-postnatal women. Journal of Affective Disorders. 39 (3), 185
Cox, J L et al. (1987) Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British journal of psychiatry: the journal of mental science. 150782
Creanga, A., Andreea et al. (2017) Pregnancy-Related Mortality in the United States, 2011
Das, Amar K et al. (2006) Depression in African Americans: breaking barriers to detection and treatment. The Journal of family practice. 55 (1), 30
Flynn, Heather A et al. (2006) Rates and predictors of depression treatment among pregnant women in hospital-affiliated obstetrics practices. General Hospital Psychiatry. 28 (4), 289
Gavin, I., Norma et al. (2005) Perinatal Depression: A Systematic Review of Prevalence and Incidence. Obstetrics & Gynecology. 106 (5, Part 1), 1071
Geier, Michelle L et al. (2015) Detection and treatment rates for perinatal depression in a state Medicaid population. CNS spectrums. 20 (1), 11
Goodman, Sherryl H. et al. (2013) Pregnant African American Women
Howell, A., Elizabeth et al. (2005) Racial and Ethnic Differences in Factors Associated with Early Postpartum Depressive Symptoms. Obstetrics & Gynecology. 105 (6), 1442
Hunt, L et al. (1989) Views of what
Kozhimannil, Katy Backes et al. (2011) Racial and Ethnic Disparities in Postpartum Depression Care Among Low-Income Women. Psychiatric Services. 62 (6), 619
Lara-Cinisomo, Sandraluz et al. (2009) Disparities in Detection and Treatment History Among Mothers with Major Depression in Los Angeles. Women
Lee King, Patricia (2012) Replicability of structural models of the Edinburgh Postnatal Depression Scale (EPDS) in a community sample of postpartum African American women with low socioeconomic status. Archives of Women
Lin, Patricia et al. (2005) The influence of patient preference on depression treatment in primary care. Annals of Behavioral Medicine. 30 (2), 164
Lori, Jody R et al. (2011) Provider Characteristics Desired by African American Women in Prenatal Care. Journal of Transcultural Nursing. 22 (1), 71
Marcus, Sheila M et al. (2003) Depressive symptoms among pregnant women screened in obstetrics settings. Journal of women
Nadeem, Erum et al. (2008) Mental health care preferences among low-income and minority women. Archives of Women
Nicolaidis, Christina et al. (2010)
Peters, Rosalind M. et al. (2014) Measuring African American Women
Salm Ward, Trina C et al. (2013)
Seng, Julia et al. (2011) Disparity in posttraumatic stress disorder diagnosis among African American pregnant women. Archives of Women
Spitzer, Robert L et al. (2006) A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Archives of Internal Medicine. 166 (10), 1092
Stevens, Natalie et al. (2018) Examining the effectiveness of a coordinated perinatal mental health care model using an intersectional-feminist perspective. Journal of Behavioral Medicine. 41 (5), 627
Woodley, Xeturah & Lockard, Megan (2016) Womanism and Snowball Sampling: Engaging Marginalized Populations in Holistic Research. The Qualitative Report. 21 (2), 321