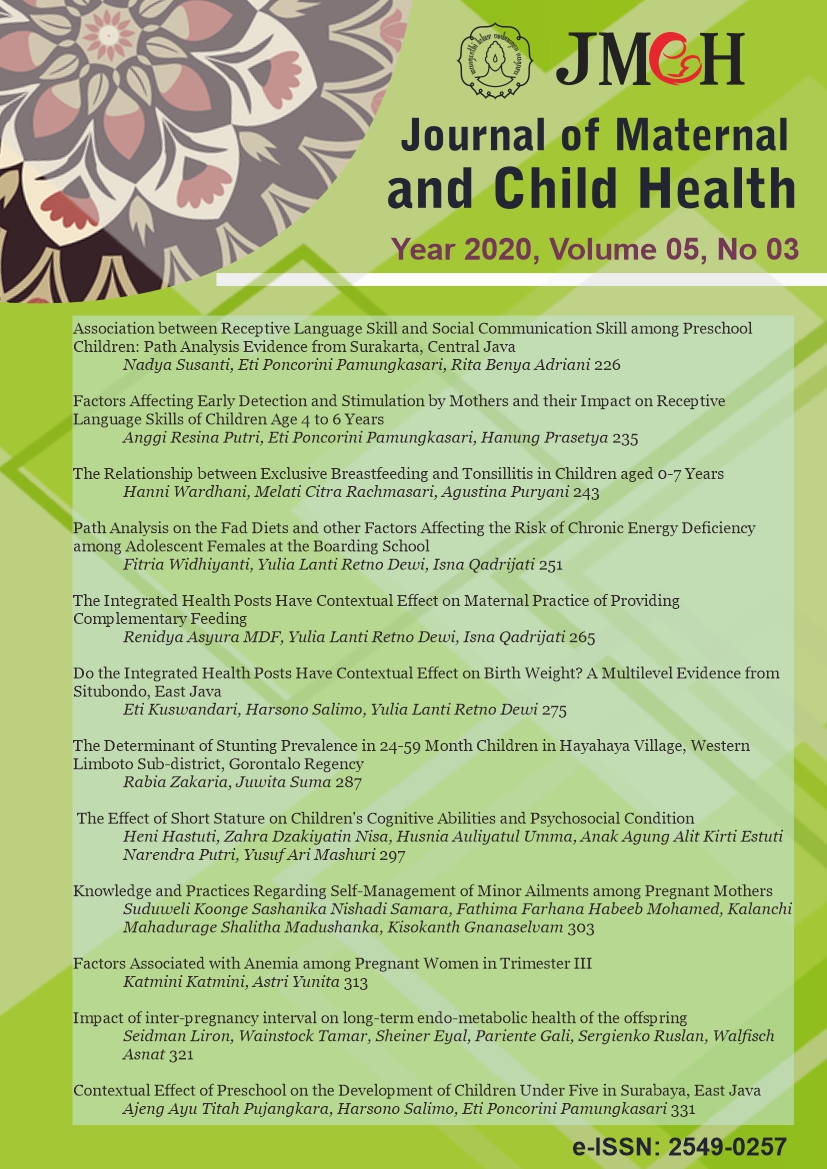
Do the Integrated Health Posts Have Contextual Effect on Birth Weight? A Multilevel Evidence from Situbondo, East Java
Abstract
Background: Low birth weight babies (LBW) are sensitive indicators of socioeconomic condi
References
Abdul A (2010). Pelayanan Kesehatan Maternal & Neonatus (Maternal & Neonate Health Services). Jakarta: Bina Pustaka
Archarya D, Singh J, Kadel R, Yoo SJ, Park J H, Lee K (2018). Maternal Factor and Utilization of the Antenatal Care Services during Pregnancy Associated with Low Birth Weight in Rural Nepal : Analyses of the Antenatal Care and Birth Weight Records
of thr. Int J Environ Res Public Health. 15(11): 1-14. http://doi.org/10.3390/ijerph15112450.
Agorinya IA, Kanmiki EW, Nonterah EA, Tediosi F, Akazili J, Welaga P, Azongo D, Oduro AR (2018). Socio demographic determinants of low birth weight: Evidence from the Kassena-Nankana districts of the Upper East Region of Ghana. PloS one. 13(11): 1
http://doi.org/0.1371/journal.poe.0206207.
Baltea P, Karmaus W, Roberts G, Kurukulaaratchy R, Mitchell F, Arshad H (2016). Relationship between birth weight, maternal smoking during pregnancy and childhood and adolescent lung function: A path analysis. Respir Med, 121: 13-20. http://doi.org/10.1016/j.rmed.2016.10.010.
D
Dinas Kesehatan Provinsi Jawa Timur (2018). Profil Kesehatan Jawa Timur (Health Profile of East Java). Surabaya: Dinas Kesehatan Provinsi Jatim. http://dinkes.situbondokab.go.id/dinkes/
Fukuda S, Tanaka Y, Harada K ,Saruwatari A, Kitaoka K, Odani K, Aoi W, Wada S, Nishi, Oguni T, Asano H, Hagiwara N, Higashi A (2017). High maternal age and low pre-pregnancy body mass index correlate with lower birth weight of male infants. Tohoku
J Exp Med, 241 (2): 117-123. http://doi.org/10.1620/tjem.241.117
Herman GH, Miremberg H, Nini N, Feit H, Schreiber L, Bar J, Kovo M (2016). The effects of maternal smoking on pragnancy outcome and placental histopathology lesions. Reprod Toxicol. http://doi.org/10.1016/j.reprotox.2016.05.022
Hartiningrum I, Fitriyah N (2019). Bayi berat lahir rendah (BBLR) di Provinsi Jawa Timur tahun 2012-2016 (Low Birth weight babies in East Java Province 2012-2016). JBK, 7(2): 97. http://doi.org/10.20473/jbk.v7i2.2018.97104
Hidayat A, Jahari A (2011). Perilaku pemanfaatan posyandu hubungannya dengan status gizi dan morbiditas balita (Utilization behavior of posyandu relationship with nutritional status and morbidity of children under five years old). Pusat Teknologi
Terapan Kesehatan dan Epidemiologi. 1
Joshi HS, Srivastava PC, Agnihotri A K, Joshi MC, Shalini CV, Mahajan (2011). Original research paper Risk Factors for Low Birth Weight (LBW) Babies and its Medico Legal Significance Abstract: Introduction: Material and Methods: Corresponding Author:
Statistical.
Kim J, Wickrama KAS (2016). Maternal social status, early health capital, and young adults
Lewis JB, Hirschi KM,Arroyo, JA, Bikma, BT, Kooyman DL, Reynolds PR (2017). Plausible roles for RAGE in conditions exacerbated by direct and indirect (Second hand) Smoke Exposure. Int J Mol Sci, 18(3): 2-22. http://doi.org/10.3390/ijms180-30652.
Maryunani A (2009). Asuhan Kegawatdaruratan dan Penyulit Pada Neonatus (Emergency care and complications in neonates). Jakarta: TIM.
Margawati AR, Widjanarko B (2016). Pengaruh status gizi & asupan gizi ibu terhadap berat bayi lahir rendah pada kehamilan usia remaja. Jurnal Gizi Indonesia, 5(1): 14-19. doi: https://doi.org/10.14710/jgi.5.1.14-19.
Mine T, Tanaka T, Nakasone T, Itokazu T, Yamagata Z, Nishiwaki Y (2017). Maternal smoking during pregnancy and rapid weight gain from birth to early infancy. J Epidemiol. Elsevier Ltd, 27(3): 112
Ministry of Health (2011). Pedoman umum pengelola posyandu (General guidelines for integrated health post managers). Jakarta: Kementerian Kesehatan RI.
Ngwira A, Stanley CC (2015). Determinants of low birth weight in Malawi: Bayesian Geo Additive Modelling. PLoS ONE, 10-(6): 1
Pantiwati I (2010). Bayi dengan BBLR (Berat badan lahir rendah) (Babies with LBW low birth weight). Yogyakarta: Nuha Medika
Paramitasari NM, Salimo H, Murti B (2018) The effect of biological, social, economic, and nutritional factors on low birth weight: A new path analysis evidence from Madiun Hospital, East Java, Indonesia. J Matern Child Health, 3: 166-175. https://doi.org/10.26911/thejmch.2018.03.03.01.
Rahayu ZB, Budhiastuti RU, Rahardjo SS (2019). Analisis multilevel determinan biopsikososial puskesmas dan modal sosial terhadap kejadin bayi berat lahir rendah di Kabupaten Lombok Timur NTB (Multilevel analysis of biopsychosocial determinants of
health centers and social capital against low birth weight babies in East Lombok Regency, NTB). J Matern Child Health, 4(3): 136-145 https://doi.org/10.26911/ thejmch.2019.09.20
Proverawati A (2010). Berat badan lahir rendah (Low birth weight). Yogyakarta: Nuha Medika
Sharma SR, Giri S, Timalsin U, Bhandari S S, Basyal B, Wagle K, Sharestha L (2015). Low birth weight at term and its determinants in a tertiary hospital of nepal A case-control study. PLoS ONE, 10(4): 1
Situbondo Health Office (2018). Profil Kesehatan Kabupaten Situbondo (Situbondo Regency Health Profile). Situbondo: Dinas Kesehatan Kab.Situbondo. http://dinkes.situbondokab.go.id/dinkes/
Situbondo Health Office (2019). Profil Kesehatan Kabupaten Situbondo (Situbondo Regency Health Profile). Situbondo: Dinas Kesehatan Kab. Situbondo. http://dinkes.situbondokab.go.id/dinkes/
Suryandari AE, Happinasari O (2016). Factors affecting the integrated health posts strata. The 4th Proseding University Research Qolloquim: 193-198.
Trisnawati I, Salimo H, Murti B (2018). Low birthweight and its biopsychosocial and economic determinants: A new evidence using a path analysis model from Jambi, South Sumatera. J Matern Child Health, 3(1): 1-10. https://doi.org/10./thejmch.2019.09.20
WHO (2014). Global nutrition target 2025 low birth weight policy brief. https://www.who.int/nutrition/publications/globaltargets2025_policybrief_lbw/en/
WHO (2017). Feto maternal nutrition and low birth weight. Geneva: WHO. Retrieved from: http://www.who.int/nutrition/topics/feto_maternal/en/(7 July 2017)
Yowono AW (2015). Pengaruh tingkat sosial ekonomi, karakteristk ibu hamil dan perilaku ibu hamil terhadap kejadian BBLR (berat badan lahir rendah) di wilayah kerja Puskesmas Lamongan tahun 2015 (Effect of socio-economic level, characteristics of pregnant
women and pregnant women behavior on the occurrence of LBW) in Lamongan Health Center in 2015). Swara Bhumi, 4(4): 53-61